Caring for Children and Aging Parents During the Holidays
The holiday season is often viewed as a time of joy, family, and togetherness. However, for those in the “sandwich generation”— adults caught between the responsibilities of childcare and caring for aging parents — this period can present unique challenges. The demands of managing the needs of a younger and older generation simultaneously can be particularly heightened during the festive season. It can be particularly challenging if you or your child have ADHD.
Read on as the Next Step team shares tips for navigating the holiday season when you’re caring for two generations.
The Holiday Stress for the Sandwich Generation
The holidays often amplify the pressures for those balancing childcare with the responsibilities of caring for aging parents. The image of a perfect holiday season can starkly contrast with the reality of these demanding caregiving roles. This leads to increased stress and feelings of being stretched too thin.
Recognizing Symptoms of Anxiety and Depression
For some individuals in the sandwich generation, the heightened stress during the holidays can trigger episodes of anxiety or depression. It’s important to be aware of signs such as persistent sadness, excessive worry, changes in sleep patterns, or a loss of interest in activities once enjoyed. Early recognition of these symptoms is crucial for effective management.
Additional reading on these topics:
- 8 Risk Factors for Depression
- 11 Ways to Help Someone with Depression
- Anxiety at Christmas
- What Is Generalized Anxiety?
The Importance of Self-Care
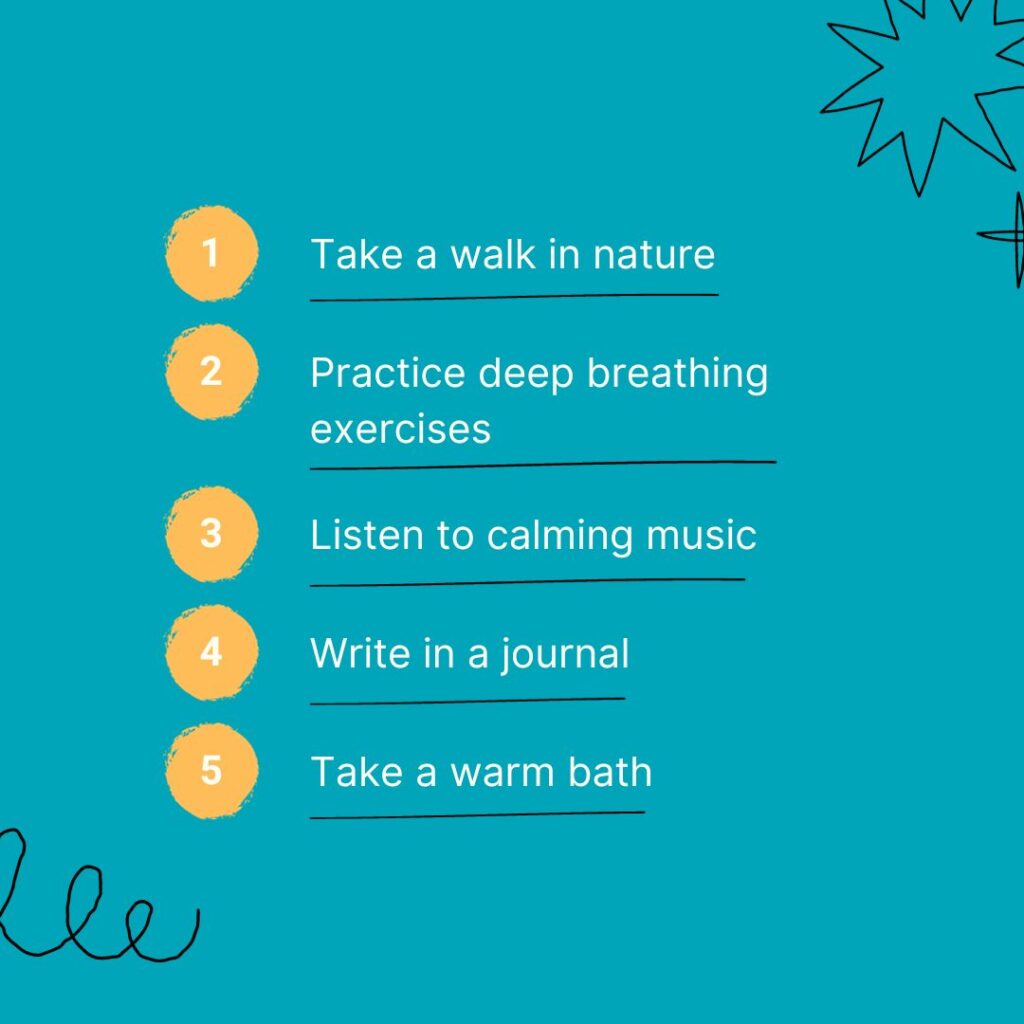
Self-care is essential for individuals juggling the dual responsibilities of childcare and caring for aging parents. Practical tips for self-care during the holiday season include:
- Setting achievable expectations
- Delegating tasks
- Setting aside ample personal time for relaxation and enjoyment
Planning and organizing can be more challenging if you have ADHD. Use as many of these tips as possible to help you stay organized.
Remember, taking care of yourself is not just a luxury, but a necessity for maintaining your overall well-being.
Click through the image slideshow for a few quick ideas to help you relax.
Additional reading on self-care:
Try a Self-Care Jar
Here’s a fun idea for the whole family to try:

Support Systems and Resources
Establishing a support network is vital. This network can comprise friends, family, and community resources. Support groups tailored for the sandwich generation or caregiver support can provide a sense of community and understanding.
Seeking Professional Help
When stress becomes overwhelming, it may indicate the need for professional assistance. Consulting with a mental health professional can provide valuable strategies for managing stress, addressing emotional challenges, and enhancing overall mental health.
The dual challenges of caring for children and aging parents during the holiday season are substantial. Recognizing when additional support is needed and taking steps to prioritize mental health are key.
Here for You
If you’re navigating the complexities of the sandwich generation this holiday season, we’re here to help. Our practice offers support, guidance, and professional assistance to help you manage these challenges. Contact us to schedule an appointment and start your journey towards a more balanced holiday season.
Learn More
The ADHD and Seasonal Affective Disorder Link
Did you know that 30% of individuals with ADHD will have a depressive episode at some point? If you have ADHD, your chances of developing depression is four times greater than it is for those people without ADHD. But how do you know if you’re dealing with major depression or seasonal affective disorder?
In this article, we’ll take a look at the ADHD and depression connection, and then we’ll zero in on the signs of seasonal affective disorder.
ADHD and Depression
In this video, Roberto Olivardia, Ph.D. explains why individuals with ADHD are more likely to experience depressive episodes.
ADHD and Seasonal Affective Disorder
There are many types of depression including major depression, seasonal affective disorder, and postpartum depression. Because fall is just around the corner, let’s focus on seasonal affective disorder.
Seasonal affective disorder, or SAD, is a type of depression that is related to the change in seasons — typically the shift from summer into fall.
You can learn more about SAD by watching the video below:
6 Signs of Seasonal Affective Disorder
Many mental health conditions share the same symptoms, so it’s important to receive an accurate diagnosis before embarking on any treatment plan. Here at Next Step 4 ADHD, our multidisciplinary team excels at diagnosing and treating co-occurring disorders.
You might suspect you have SAD if you:
- Feel sad
- Notice changes in your sleeping and eating patterns
- Have lost interest in your favorite hobbies
- Feel more intensely sad with the changing of the seasons
- Feel guilty
- Feel worthless
- Suicidal thoughts
The National Suicide Prevention Lifeline is a national network of local crisis centers that provides free and confidential emotional support to people in suicidal crisis or emotional distress 24 hours a day, 7 days a week.
Their number is 1-800-273-8255.
Treating SAD and ADHD

The good news is that the right treatment can help you feel better. SAD is often treated with lifestyle modifications (exercise, sleep hygiene, spending time outside), therapy, and medication.
Don’t brush off these symptoms. If you’re struggling with feelings of sadness, and you suspect that you might have ADHD and SAD, don’t hesitate to reach out to us. You can reach our Louisville, Kentucky office at 502-907-5908. You can also request an appointment online.
Learn More
Seasonal Affective Disorder and ADHD: 4 Tips to Fight Depression
Do shorter days and darker nights have you feeling a little blue? Seasonal affective disorder (SAD) is common during the darker winter months, and unfortunately, SAD disproportionately affects individuals with ADHD.
If you’re experiencing any symptoms of SAD, we recommend that give us a call. Whether you’re struggling with SAD, depression, or ADHD, we can help you.
In the meantime, keep reading to explore what SAD is and how you can keep it at bay.
ADHD and SAD
Like depression, SAD is a mood disorder. It is associated with depression and related to seasonal changes in light. In countries where the sunlight hours are few (such as the Nordic countries), SAD impacts up to 20% of the population.
Even beyond the icy dark Nordic countries, SAD may disproportionately affect adults, teens, and children who have been diagnosed with attention deficit hyperactivity disorder (ADHD). Researchers estimate that 27% of the individuals with ADHD also struggle with SAD — that’s 7% more than those already living in darker climates.
What Is Seasonal Affective Disorder?
Seasonal affective disorder is a type of depression that is triggered by the change of seasons and the variations in hours of daylight each day.
Most people with SAD notice their symptoms begin in autumn and extend through the winter.
Symptoms of SAD (whether or not you have ADHD) include:
- Increased feelings of sadness
- Feeling depressed almost every day
- Loss of passion for your favorite activities
- Fatigue and low energy levels
- Difficulty sleeping
- Changes to your appetite
- Feeling agitated
- Trouble concentrating
- Experiencing feelings of hopelessness or guilt
- Having frequent thoughts of death or suicide
Why Do Variations in Light Affect Your Mood?

Why do the changing seasons affect your mood? Here are three contributing factors:
- Your circadian rhythm: Decreasing sunlight may disrupt your body’s circadian rhythm. If your internal clock is impacted, it can lead to feelings of depression.
- Serotonin levels: Reduced sunlight can also cause a drop in serotonin, and this decrease in serotonin may trigger depression.
- Melatonin levels: The change in sunlight doesn’t just affect your serotonin levels. It can also impact your level of melatonin. Changes in melatonin can alter your sleep patterns and even your mood.
4 Tips for Reducing the Impact of Seasonal Affective Disorder
Now that we’ve covered what SAD is, how to spot the signs of SAD, and how light affects your mood, what can you do about it?
Here are four strategies you can implement.
1. Schedule Regular Exercise
If you spend less time outside during the winter, you’re not alone. Most people naturally spend less time outside during the winter because #brrr.
And less time outside often equates with less physical activity, and that can definitely impact your mental health.
Most people spend only 7.6% of their time outside. Considering that Americans also spend 5% of their time simply driving in the care, 7.6% isn’t a whole lot!
The changing weather, the decreasing light, and the decrease in physical activity is a perfect storm. If you think you have SAD or depression, consider scheduling regular exercise into your day.
Moving your body promotes good brain chemistry, which can help you feel better.
The Norwegian have a wonderful proverb: “There’s no such thing as bad weather, only bad clothes.” Bundle up and try some cold-weather activities like skiing, cross-country skiing, or snowshoeing. Even a leisurely stroll in the brisk air is good for you.
Prefer to say in? No worries! There are plenty of indoor activities to keep you active: running on a treadmill, yoga, Pilates, lifting weights, or following along on YouTube dance workout.
2. Soak Up Some Sunshine

Even if the sunlight diminishes, try to soak up a little sunshine each day. Research shows that low vitamin D levels can contribute to SAD. Experts suggest trying to get 30 minutes of morning sun — to start the day off right. If you go for a jog or walk at this time, you’ve crossed two items off of this list at once: regular exercise and time spent outside.
3. Stick with Your Schedule
Sleep disturbances are common with SAD. In order to prevent even more sleep interruptions, stick with a schedule.
- Go to sleep at the same time every night
- Avoid blue lights before bed
- Sleep in a cool, dark room
You can find more sleep tips in this article: What Is Sleep Hygiene?
4. Seek Treatment
Even if you’re exercising regularly and getting to bed on time, SAD can still take root.
If you are experiencing symptoms of SAD during the fall or winter months, contact one of our mental health professionals who can help you “weather the storm.”
Call our office at 502-907-5908 or request an appointment online.
Learn More
Is It Burnout or Something Else? Helping Healthcare Workers and First Responders Understand Compassion Fatigue
Given the high-stress environment that includes packed workdays, time pressure, and emotional intensity, it is a common experience for first responders and healthcare workers to experience burnout. You might even use this phrase yourself, but what does it really mean to be burnt out? And more importantly, is there something else going on besides burnout?
In this post, we’ll cover:
- What burnout is
- Why first responders need to know the signs of compassion fatigue
- What to do if you’re burned out
Burnout or Compassion Fatigue?
Burnout is defined as a long-term stress reaction that is marked by physical exhaustion and a feeling of a lack of accomplishment [2].
Nearly anyone in a stressful situation can experience physical and mental symptoms of stress, physical exhaustion, and a lack of sense of accomplishment. However, because their work frequently puts them in a position to see unimaginable suffering, it is not unusual for healthcare providers and first responders to experience these symptoms in excess. This is called compassion fatigue. Some first responders and healthcare workers even absorb the emotional stress and trauma of those people that they are helping.
This is especially true in the current care environment created by the concurrent pandemic and community unrest.
Many healthcare workers and first responders have begun filling a dual role to their patients: care provider and emotional support person. Many care providers are filling in for families, who are unable to be a part of their loved ones’ final moments, to provide comfort and support. This type of emotional investment and compassionate care places them at increased risk of compassion fatigue.
However, given the current need for long hours, increased number of shifts, and increased workload during shifts, many providers mistake symptoms of compassion fatigue for simple burnout. Denial is perhaps the most detrimental symptom of compassion fatigue, as it leads providers to not seek help due to believing that they are simply exhausted [1].
Signs and Symptoms of Compassion Fatigue
Denial is a detrimental symptom of compassion fatigue, but it’s not the only symptom. Some common symptoms of compassion fatigue include the following:
• Feeling burdened by the suffering of others or blaming others for their suffering
• Isolating yourself
• Loss of pleasure in life
• Irritability or sadness
• Difficulty concentrating
• Insomnia
• Physical and mental fatigue
• Physical ailments, such as headaches or stomachaches
• Feeling that you have no outlet for your emotions
• Increased nightmares
• Feelings of hopelessness or powerlessness
• Decreased job satisfaction
• Overeating or poor appetite
• Excessive use of drugs or alcohol
• Decreased or poor self-care
• Complaints from others about your work or attitude
• Denial
How to Check-In With Yourself: Are You At Risk?
If you are a healthcare worker or a first responder, it’s important to check in with yourself and watch for signs of compassion fatigue. You can recover from burnout and compassion fatigue, but it’s best to catch it early, if possible.
Some questions to ask yourself:
• Is my stress getting in the way of living my life (Is my daily functioning altered?)?
• Did a work experience feel out of the ordinary or feel like it overwhelmed my ability to remain calm and neutral?
• Do I find it hard to separate from work once the shift/workday is over? Do thoughts and memories of my day impinge upon my time off?
• Do I feel like I accomplish less during the day, even when I feel like I am working harder?
• Do I find myself becoming easily frustrated, irritated, or annoyed, especially in response to situations or triggers that previously did not elicit such a strong reaction?
• Do I experience compassion in the extremes (i.e. little or no compassion toward some people while becoming overly involved with others)?
• Do I find myself feeling bored or disengaged from my work?
• Do I find myself suffering from mild physical ailments, such as headaches or minor colds, more frequently than before?
WHAT YOUR ANSWERS MEAN: If you answered yes to any of the above questions, you may be suffering from compassion fatigue rather than burnout.
As a caregiver, it is vital that you find balance between care for others and care for yourself. Placing more focus on others places you at increased risk of compassion fatigue; however, caregivers frequently struggle to know how to care for themselves.
8 Ways to Restore the Balance in Your Life
Below are some tips for how to find and keep balance in your life.
1. Practice self-care.
Good self-care involves taking care of your physical, emotional, and spiritual health. Make sure to eat well, drink plenty of water, exercise regularly, and get plenty of sleep. Do not allow yourself to become isolated. Make time to engage in social interactions with people with whom you do not work. Ask yourself daily who is one person that you could reach out to and call them. If applicable, continue to attend religious worship services. Gatherings of your religious community are helpful in finding a continued sense of purpose and support.
2. Make sure to nurture yourself.
Find time daily to engage in activities that are a source of pleasure and distraction from the stresses of your day. Make this self-nurturing time a priority. It may be helpful to make a top 10 list of activities that bring you joy.
3. Allow yourself to take multiple mini-breaks during your workday.
Take a walk, leave the premises on your meal break, or just sit in your car for 15 minutes. It is important to take short escapes from the stresses of your workday.
4. Attempt to divert focus away from the negatives of the work and focus on the positive impact of your work.
Find what brings purpose and meaning to your job and find the things that you are grateful for.
5. Focus on what you can control and try to let go of things that you cannot control.
Write it down on paper if that helps you to visualize it.
6. Find someone to talk to and with whom you feel that you can share your pain and suffering.
However, avoid commiserating with coworkers. In this situation, misery does not love company.
7. Avoid self-medication with drugs and alcohol.
If symptoms are impairing your functioning (i.e. poor sleep), seek out professional medical treatment to address these concerns.
8. Seek out professional help.
Many people who are suffering from compassion fatigue need the help of professional coaches, counselors, or therapists to get back on track. Many employers have employee assistance programs just for this purpose. Find out what services your employer and/or insurance provider offers.
We’re Here to Serve You
About the Author
 This post was written by Monica Clark, LPA.
This post was written by Monica Clark, LPA.You can request an appointment with Monica here.
References:
- Bourg-Carter, Sherrie. 2014. High Octane Women. Psychology Today. Retrieved from
https://www.psychologytoday.com/us/blog/high-octane-women/201407/are-you-suffering-compassion-fatigue - Physician Burnout. Content last reviewed July 2017. Agency for Healthcare Research and Quality,
Rockville, MD. Retrieved from https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html